Failed MVD for TGN: Confusing Anatomy
Fothergill’s disease or trigeminal neuralgia is considered one of the worst pains that can affect a human being. The severity of this disabling pain and its relief through successful operative intervention have caused microvascular decompression (MVD) surgery to be recognized as one of the most satisfying operations in neurosurgery.
A middle aged male was presented to us with history of episodic Left sided lancinating facial pain in V2 and V3 distribution of Trigeminal Nerve. He underwent MVD one month ago. But pain did not settle.
Re exploration was performed by senior surgeon. During surgery adhesions were present in superior complex of Cerebellopontine fissure, but no adhesions were present at 5th nerve root entry zone area. Unusual low position of 4th nerve led to previous surgeon false perception of 5th Cranial nerve. Following second surgery patient’s pain relieved.
Pathological Anatomy for TGN
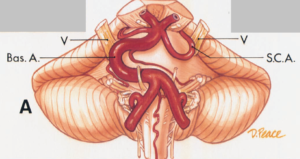
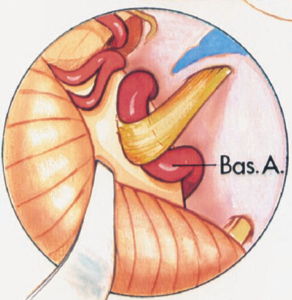
The most common finding at a vascular decompression operation for trigeminal neuralgia is a segment of the SCA compressing the trigeminal nerve. Normally, the SCA encircles the brainstem well above the trigeminal nerve.
In adults, the SCA commonly makes a shallow, caudal loop and courses inferiorly for a variable distance on the lateral side of the pons . In those cases with the most prominent caudally projecting loop, contact between the artery and the trigeminal nerve occurs. The point of contact with the SCA is usually on the superior or superomedial aspect of the nerve.
The medial axilla of the nerve must be carefully explored before concluding that there is no arterial loop in the axilla of the nerve. The SCA gives off perforating arteries that may limit the degree of repositioning of the artery achievable in a microvascular decompression operation.
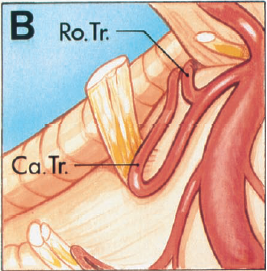
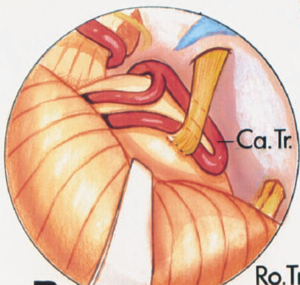
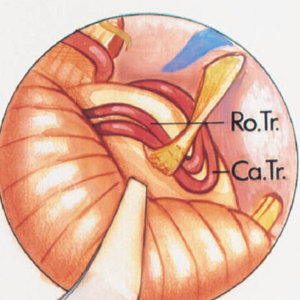
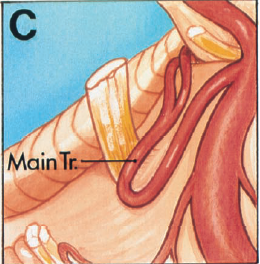
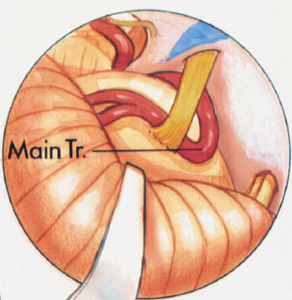
The most common site of compression of the trigeminal nerve on the SCA is at the junction of the main trunk with the origin of the rostral and caudal trunks .
Alternatively, if the artery bifurcates before reaching the nerve, the caudal trunk may compress the nerve and the rostral trunk may course well above the nerve.
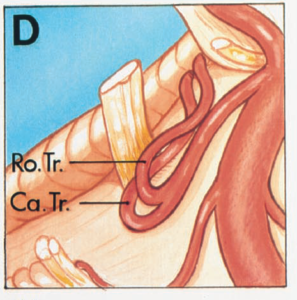
If the artery bifurcates distal to the nerve, only the main trunk will be involved in the compression. The point of bifurcation of the SCA does affect the caliber of the vessel that makes contact with the nerve. The contacting vessel will be of a smaller caliber if the SCA bifurcates before reaching the trigeminal nerve.
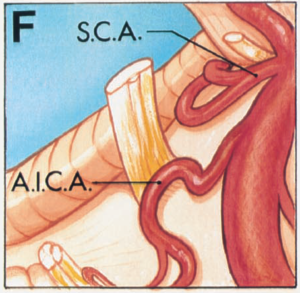
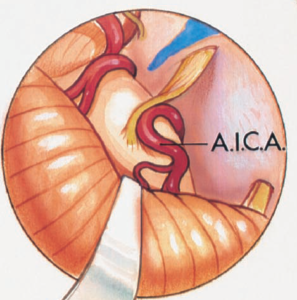
A less frequent source of compression of the trigeminal nerve is by the AICA. Normally, the AICA passes around the pons below the trigeminal nerve with the facial and vestibulocochlear nerves.
The AICA, however, may have a high origin and loop upward to indent the medial or lower surface of the trigeminal nerve before passing downward to course with the facial and vestibulocochlear nerves.
A serpentine basilar artery also may wander laterally and compress the medial side of the trigeminal nerve. This type of basilar artery often is elongated and has a fusiform configuration.
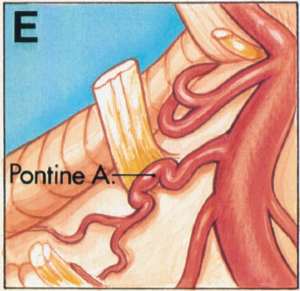
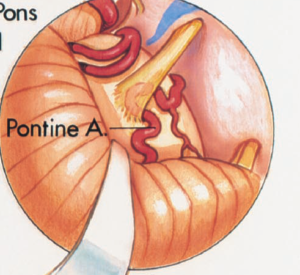
More than one artery may compress the nerve. In a few cases, the SCA will compress the rostral surface of the nerve and the AICA will compress the caudal surface. Infrequently, the posteroinferior cerebellar artery (PICA) may reach and groove the undersurface of the trigeminal nerve. The trigeminal nerve also may be compressed by a large pontine branch of the basilar artery
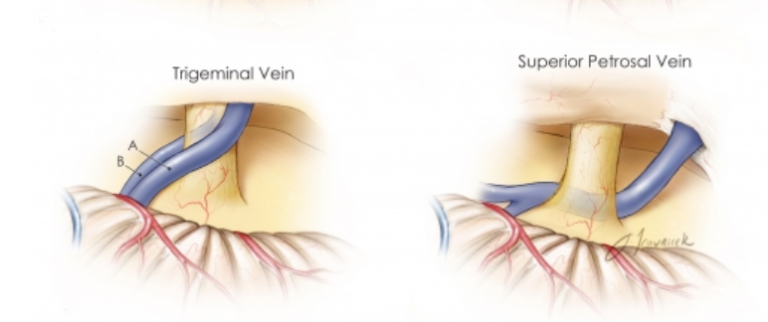
Compression and distortion of the trigeminal nerve by the surrounding veins, although less frequent than arterial compression, also is found in trigeminal neuralgia.
It is the superior petrosal veins that empty into the superior petrosal sinus that are most frequently encountered in operative approaches to the trigeminal nerve and that most commonly compress the trigeminal nerve.
The most common tributaries of the superior petrosal veins are the transverse pontine and pontotrigeminal
veins, the veins of the cerebellopontine fissure and the middle cerebellar peduncle.