Anterior Communication Artery Aneurysm Clipping: Left versus Right Pterional Craniotomy
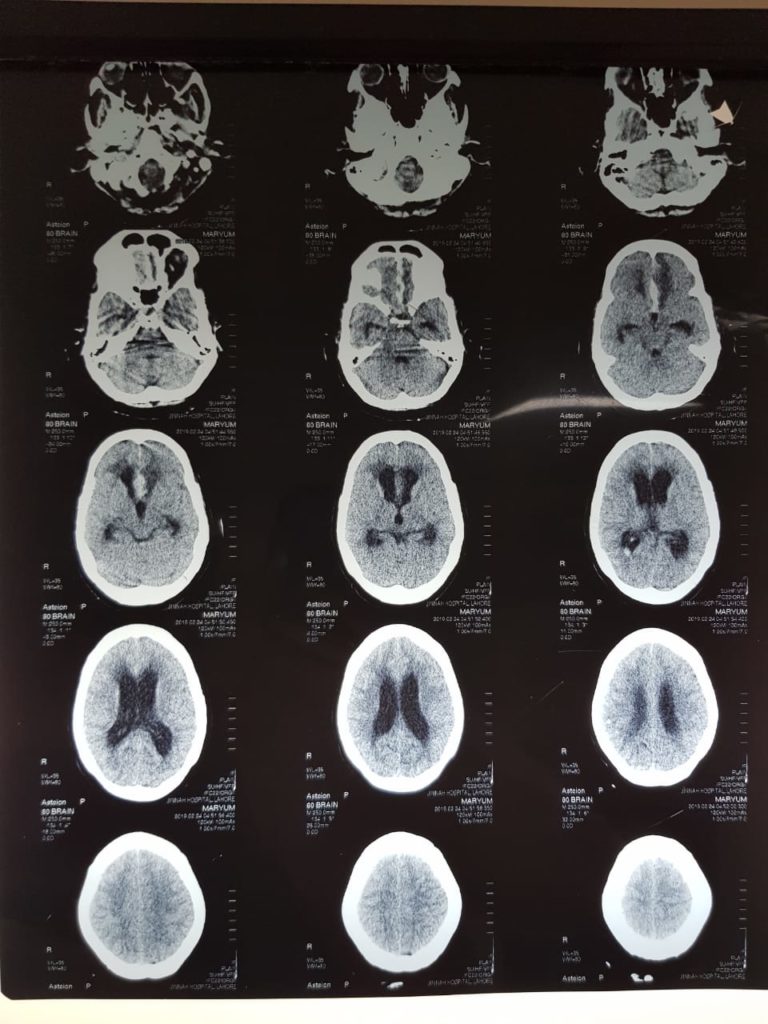
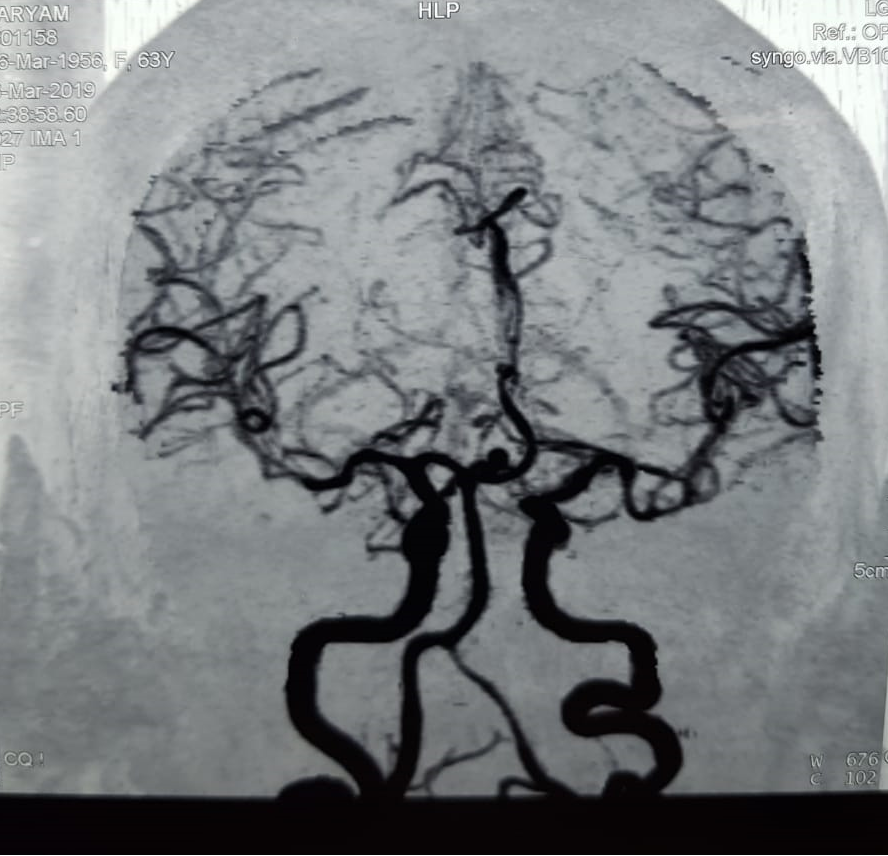
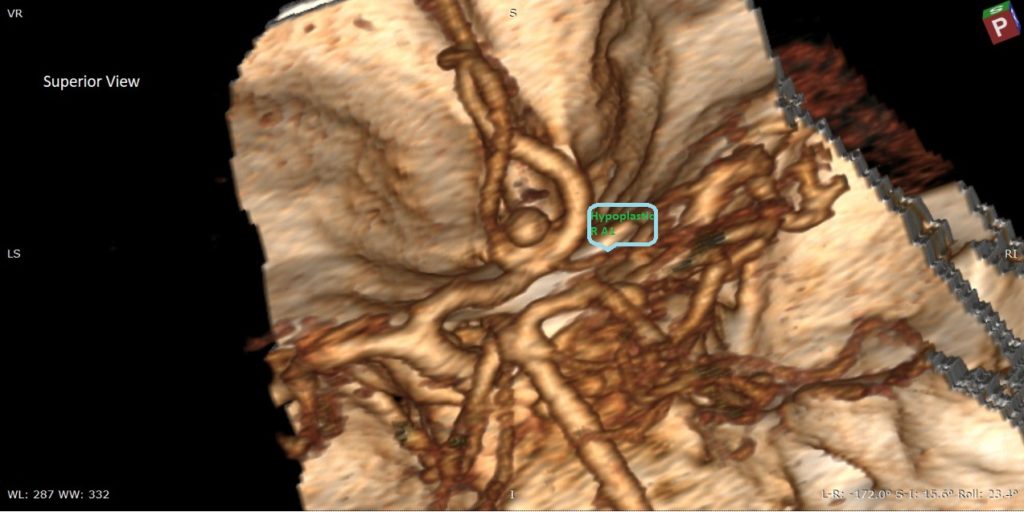
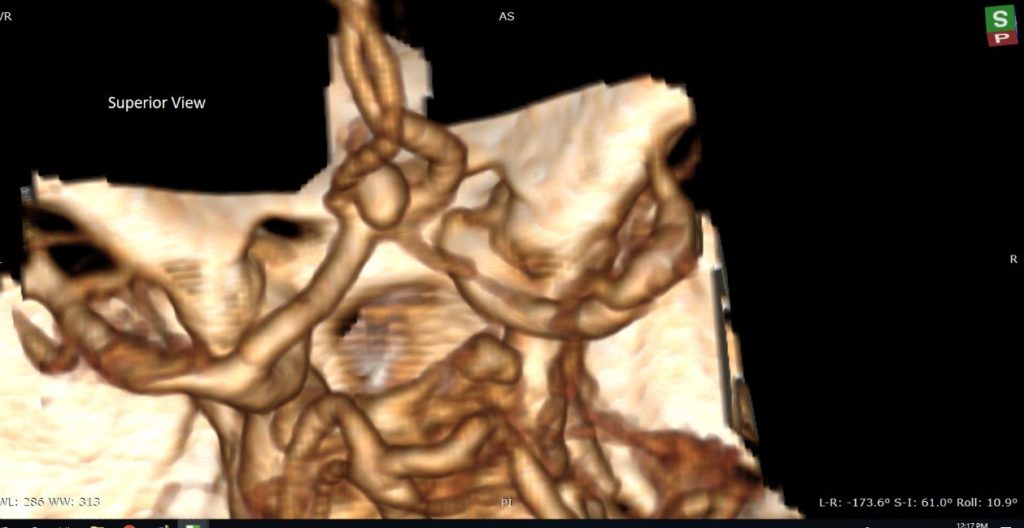
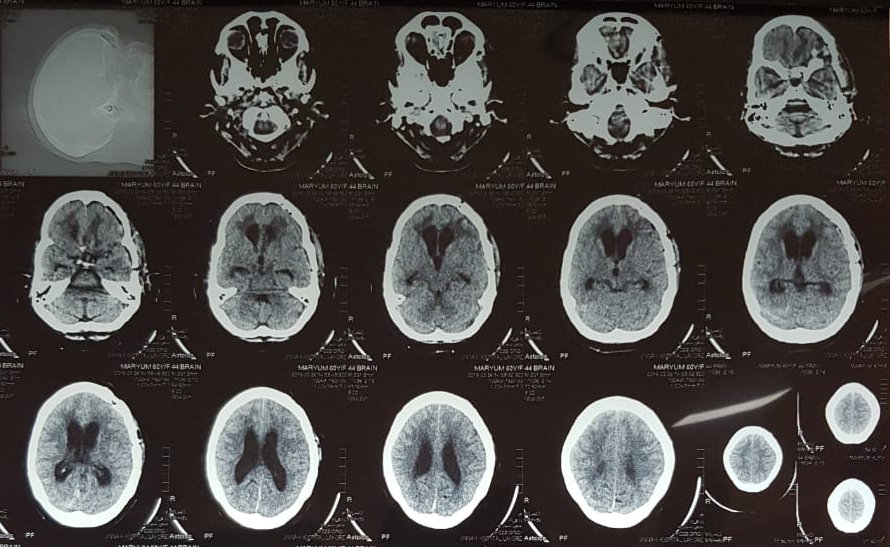
A 60Y/Female was presented in Medical Emergency with sudden altered conscious level and vomiting. On Examination her GCS was 12/15 with neck rigidity. CT Scan Brain was done and showed Subarachnoid Hemorrhage. She was consulted by neurosurgery team and found WFNS grade II. She was shifted to Neurosurgical High Dependency Unit. Later her C.T angiography showed Superio-posterior directed aneurysm of anterior Communicating artery (A com A). She was offered both coiling and clipping. Her family opted for clipping (mainly due to cost factor, at our institution clipping is free of cost).
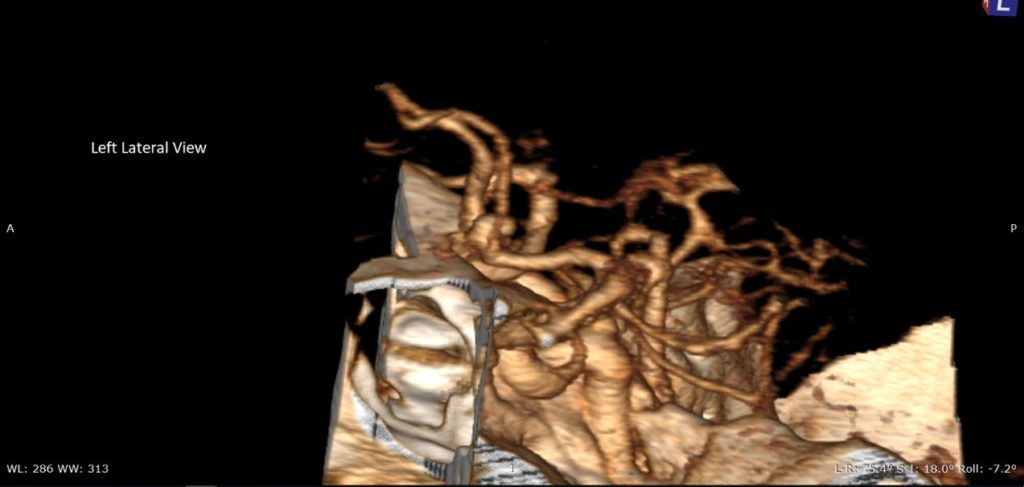
Left Pterional Craniotomy was planned due to hypoplastic right A1 segment of ICA.
Discussion
The history of intracranial surgery for aneurysms is not a long one. The first direct operation on an intracranial aneurysm was performed by Norman Dott, who wrapped a ruptured aneurysm in 1933, and the first obliterative clipping of an aneurysm was performed by Walter Dandy in 1938. The results of surgery improved dramatically when the operating microscope was introduced in the 1960s and a subsequent improvement followed the use of the calcium antagonist nimodipine and the maintenance of a high fluid intake to lessen the risk of delayed cerebral ischaemia.
For many years clipping of a ruptured aneurysm was regarded as the definitive mode of treatment, but the development of the GDC coil in 1990 allowed an alternative approach that avoided the hazards of open surgery. In the latter half of the 1990s, as experience of endovascular techniques spread, this form of treatment began to displace open surgery and the International Subarachnoid Aneurysm Trial (ISAT) was set up to compare the efficacy of the two forms of treatment and showed early safety of coiling over clipping.
In Pakistan there is also gradual increase in trend towards coiling. But there is one factor still important for decision making, is cost issue. Surgery for clipping an aneurysm is almost free in public sector hospital but coils has to be purchased by patients by their pocket. Still art of clipping be applicable in our country.
There are two main types of approaches for anterior communicating artery (AcomA) aneurysms, namely pterional approach and an interhemispheric approach. A pterional approach is the most common for aneurysm surgery, not only for anterior circulation aneurysms but also for basilar tip aneurysms.
The pterional approach has the following advantage: the subarachnoid space is widely opened and the hematoma can be removed as much as possible in the acute stages of SAH; damage of the olfactory nerve is minimized and bilateral parent arteries of the proximal side can be secured in early stage of the procedure. As a disadvantage, the brain must be compressed, and partial resection of the gyrus rectus is often required in cases of high-positioned anterior cerebral artery (ACA) aneurysms.
Determinants of the Approaching Side
The determining factors include
A1 predominance
direction of A2 fork
the direction of the aneurysm
the size of the aneurysm
and multiplicity of the aneurysms.
The presence of fenestrations of the AcomA is an important factor in determining the side of approach.
In cases of acute SAH, determining factors include the distribution of SAH and ICH.
In case of small and large sized aneurysms directed anteriorly), the A1 dominance should be the most important factor, because it is sometimes difficult to secure the opposite side of A1. But there is no marked difference in surgical difficulty between the right and left approaches.
In the case of aneurysms directed superiorly, the A1 is bilaterally secured before approaching the aneurysm. Therefore entry into the open part of the A2 (i.e. the side of A2 facing posteriorly) facilitates clipping .
In cases of aneurysms directed postero-inferiorly and located at the back of the AcomA, entry through the side of the A2 located more anteriorly is recommended, as if the posterior surface of A2, especially in cases of fenestration of the AcomA.
Giant aneurysm is, as a rule, treated by an approach from the direction in which early arrival at the aneurysm neck is accomplished. Approaching from the side of dominant A1 is generally recommended.
References:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC539625/
https://www.wfns.org/WFNSData/Document/ClinicalResources/Anterior_Communicating_Artery_Aneurysms.pdf